
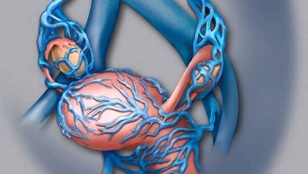
Both men and women are susceptible to varicose veins, but members of the weaker sex often suffer from the consequences of this disease. Often, the compounds associated with varicose veins occur with swelling of the veins in the legs below the knee, but in women there is something like varicose veins of the small pelvis. It is a very common disease that affects all women during childbirth.
Varicose veins in the small pelvis often occur in women who do heavy physical work or during pregnancy. This is due to increased stress on the female body, which leads to an increase in venous pressure, which in turn stimulates the varicose veins of the hip.
Sudden pain in the lower abdomen is the first symptom of varicose veins in the small pelvis.
Varicose veins of the internal organs are especially dangerous for pregnant women and are one of the main reasons for prescribing a caesarean section. Doctors explain this by the fact that natural childbirth can cause bleeding and endanger the lives of mother and child. Occurrence of this disease during pregnancy is due to the fact that the enlarged uterus is compressed and interferes with normal blood circulation. Increased hormone levels are also a factor in the formation of varicose veins in the small pelvis.
Due to changes in hormonal levels in adult women, the disease may begin to develop during adolescence. The situation is complicated by the fact that varicose veins of the pelvic vessels are very difficult to detect, because the disease, which occurs during this life, rarely continues with obvious symptoms. An indirect reason to consult a specialist may be increased discharge in the organs of the female reproductive system.
Often, varicose veins of the small pelvis in women occur while sitting in the office. This is because a person loses the plasticity of the venous walls due to low mobility. Men are also susceptible to this disease, but less so than women.
The most obvious symptom of varicose veins of the small pelvis may be more frequent pain in the lower abdomen, especially when the body is upright. Often, the pain is caused by sexual intercourse or other intense stress on the body. Varicose veins from the small pelvis can spread to the perineum and gluteal region.
Experts call the internal varicose veins of the small pelvis a complex disease. This is due to difficulties in diagnosis, because the initial symptoms of the disease are not so many and they do not manifest themselves clearly. Timely detection of varicose veins gives hope for complete recovery. There is a high probability of misdiagnosis in the early stages of the disease.
The main causes of the disease

Poor heredity can be a problem.
Dysplasia of connective tissues is a precursor to pathologies of the pelvic vessels that cause varicose veins. Often these problems are due to poor heredity, but people whose lives are associated with the following factors can also suffer from varicose veins:
- Office work or other sedentary occupation;
- Heavy physical activity, if the body is not prepared for them in advance;
- Irregular sexual activity;
- High estrogen hormone;
- Gynecological diseases of women, frequent inflammation;
- Tumors located near the internal organs.
Studies have shown a link between the use of contraceptives and other hormonal medications in the formation of varicose veins in the small pelvis.
Coverage of this disease in pregnant women requires special attention. Unfortunately, in all cases, up to 30% of women have the disease during this period. Doctors believe that pregnancy can trigger connective tissue dysplasia, which causes varicose veins in a woman's body.
In women, varicose veins of the small pelvis occur due to an increase in the number of female hormones in the body, the effect of which is similar to the use of contraceptives. This is aggravated by the fact that during the development of the fetus, it puts pressure on the internal vessels of the pelvis and causes compression. After childbirth, additional pathways for unwanted blood flow occur, and a recovery procedure is required to eliminate them.
For those who are registered, there is a risk group in the antenatal clinic that includes women prone to inflammation of the reproductive organs. Pregnant women with high estrogen levels also require special attention.
Symptoms of the disease

The main symptoms of pelvic varicose veins include more frequent pain in the lower abdomen and excessive discharge of mucus from the genitals. However, there may be other causes of these symptoms, which is why it is so difficult to diagnose such varicose veins of the small pelvis in the early stages.
Indirect symptoms include swollen arteries in the thigh and perineum. In some patients, lower abdominal pain increases in the first days of the menstrual cycle.
The main symptoms of pelvic varicose veins in women are:
- Pain before menstruation is stronger than ever;
- Menstrual disorders;
- Strengthening of sensations in the perineal region;
- Pain from the lower abdomen to the lower back;
- Increased vaginal sensitivity;
- Frequent urination;
- Violence in the lower back when standing or sitting for long periods of time.
Depending on the stage of development of small pelvic varicose veins and the individual characteristics of each woman, several symptoms can be observed at once, or each separately. In any case, if any of the listed symptoms are found, you should visit the gynecologist's office.
Diagnostic methods
There are several methods for detecting and diagnosing varicose veins of the pelvic organs, but Doppler ultrasound is the main method. When using this procedure, it is possible to determine the contours of the vessels with ultrasound waves and display them on the screen of the device or take a photo. The image allows you to detect all areas of deformation in which the blood flow in the vessels is reduced.

For a clearer picture, doctors use phlebography in diagnosis. The uterine vessels are filled with a substance that gives contrast during fluoroscopy.
The difficulty in diagnosis is the absence of a certain localization area, varicose veins in the small pelvis, along with mild symptoms.
When diagnosed by a doctor, varicose veins can be confused with a widespread inflammatory process, the likelihood of such a mistake is particularly high in the early stages.
Important!If a gynecologist diagnoses inflammation and prescribes therapy, but it does not help to cope with the symptoms, it is important to understand that such an effect is not normal, and it is important to consult a specialist a second time.
You can rely on the following methods to make a correct diagnosis:
- Doppler ultrasound;
- Phlebography - makes a fairly accurate diagnosis of varicose veins of the small pelvis;
- Ultrasound examination of the venous system - vaginal examination or transabdominal scan is used in various situations;
- Laparoscopy - this method can also detect the formation of varicose veins in the ovaries;
- Selective ovarycography - this diagnostic method is likely to detect varicose veins in the small pelvis. To do this, contrast fluid is injected into the veins of the thigh and subclavian region.
If the diagnosis does not give accurate results, the patient may be referred for additional examination. A blood test is scheduled.
Classification of disease severity
Pelvic varicose veins can be divided into three categories depending on the stage and severity. An important parameter in this regard is the location of varicose veins.
- In the first stage, the varicose veins in the small pelvis swell up to 5 mm due to the appearance of a small number of deformed areas;
- In the second stage, the vessels are between 6 and 10 mm in diameter, and an empty ectasia of the plexus occurs in the ovary;
- Extremely dangerous, the patient's venous swelling is more than 10 mm in size. The third degree of lesion is characterized by parametric localization of the main type.
After a successful diagnosis and determination of the stage of the disease, appropriate treatment of varicose veins is prescribed.
Conservative treatment methods

Once a correct diagnosis has been made, it is best to contact the appropriate specialists. Diseases associated with varicose veins are treated by a phlebologist. You can only consult a gynecologist after being diagnosed and confirmed by a urologist for pelvic vascular dilatation in men.
The main tasks that set the doctor on the patient's recovery are:
- Restoration and restoration of damaged vascular walls;
- Prevention of further blood stasis in small pelvic vessels;
- Improving the condition of vascular tissue.
To solve the set tasks, a special diet, rehabilitation exercises, drugs for the treatment of varicose veins and a complex therapy, which includes the use of underwear that gives a special shape, are used.
Therapeutic phase of treatment
The main goal of therapy for small pelvic varicose veins is to restore blood flow and normalize elastic tissue tone. The stages of eliminating the unpleasant symptoms of the disease and increasing blood circulation in the arteries are also important.
Preparation for varicose veins should be prescribed only by a phlebologist. There are two groups of drugs prescribed for this disease. The first (venotamic drugs) - improves the tone of vascular tissues, the second (angiagregants) - prevents new blood clots.
In case of exacerbation of varicose veins of the small pelvis, taking medication is an important part of therapy. The main role in treatment is given to venotonic drugs that improve vascular tone. These drugs are prescribed for prophylaxis to prevent recurrence of the disease.
Preparations for the treatment of varicose veins of the small pelvis can be prescribed only by a doctor, self-medication is unacceptable!

In general, varicose vein medications help:
- Stop the backflow of blood;
- normalization of venous tone;
- help blood supply to tissues;
- Reduce anxiety from the symptoms of the disease.
Remember that medication should be combined with special exercise and a prescribed diet.
Traditional medicine
For the treatment of varicose veins of the small pelvis are often resorted to folk remedies, among which the main methods are herbal infusions that restore the normal tone of the veins. The most popular decoctions are horse chestnut, chaga and dandelion roots.
Hirudotherapy has proven itself well in humans: the bones should be applied to the sacrum and coccyx.
Important to know!It is impossible to allow varicose veins found in the small pelvis to slip or to rely only on traditional medicine. This extremely dangerous disease must be treated comprehensively with mandatory medication, and the use of infusions and decoctions can only be an additional tool.
Preventive gymnastics
There are several ways to exercise to restore tissue tone.
- Raising and lowering the toes, training standing, number of repetitions at least 30, toes and ankles parallel;
- The same thing, just separate the socks and straighten the heels 30 times;
- Repeat the toe lift, bringing the toes together, spreading the heels to the maximum;
- Pelvic varicose veins can be treated with breathing exercises by slowing down by imagining how all the abdominal muscles are involved;
- In a prone position, lift the pelvis with your hands and do a "bicycle" movement, for those who find it difficult to do, you can replace or replace them with "birch".

If the veins of the small pelvis dilate, physiotherapy is a good exercise, it is convenient to do anywhere. The main condition for success will be the regularity of special exercises, but under no circumstances should you strain yourself too much during the lessons.
If venous dilatation is diagnosed, it is equally important to follow a healthy lifestyle. You should take regular breaks during physical activity, and if it is associated with staying in a static position for a long time, you should take breaks from time to time, warm up and walk.
A good solution would be to use a contrast shower, as varicose veins cause discomfort in the perineal area, so it is no longer possible to direct the flow of water to this area.
Proper nutrition
It is important to develop a diet so that there are no problems with stool, especially constipation. Thus, venous dilatation may be aggravated by an increase in internal pressure during bowel movements. It is better to exclude very spicy and fatty foods, as they affect the formation of blood clots.
Nutritional correction of pelvic varicose veins involves the exclusion of foods containing saturated fat and any alcoholic beverages. Preference should be given to dietary fiber foods (vegetables and fruits, cereals), healthy fats (vegetable oils).
After learning from your doctor how to treat varicose veins of the small pelvis and what dietary restrictions to apply, you should look at the general condition of the body, it is better to give up bad habits (smoking and alcohol) during rehabilitation.
Possible complications
Varicose veins of the pelvic organs can cause serious complications in the female body, especially in the later stages of the disease. Sometimes the inflammation spreads to neighboring organs, and uterine bleeding appears more frightening.
For better protection, you need to understand the dangers of pelvic varicose veins. Frequent bleeding in the uterus can lead to thrombosis and become a widespread inflammatory process.
Forecasting
In women, varicose veins of the small pelvis can contribute to the development of serious consequences, but in most cases they occur in the later stages due to the late detection of the disease. Therefore, you should pay attention to the pain with pelvic varicose veins, as these are the most obvious symptoms that indicate the need to consult a doctor.























